As Time Goes By: Ageing in Staffordshire
Director of Public Health Annual Report 2024
Foreword
The UK’s population is ageing. The first half century after the turn of the millennium will see a substantial change in our demographic profile - with many more older people and a relative reduction in the number of working age adults. This will have profound consequences for how we organise our society and our public services, with health and care services particularly affected.
This Director of Public Health Annual Report provides some key data to highlight the way that the population is ageing. The aim is to help local organisations understand and take account of this demographic change. My hope is that the Report might facilitate a ‘silver thread’ through local strategy and policy - for the environment, the economy, housing, policing, and of course health and care.
The Report explores the potential impact of the ageing population on health and care services in more detail. The aim is not to produce precise estimates of the additional financial and human resources that will be required, nor to analyse these in detail by sector and service. The aim instead is to provide some headline figures to illustrate a point and stimulate a conversation.
The point is this: as things stand, health and care services are going to need a lot more funding and a lot more staff over the next 20 years, and it is difficult to see where these are going to come from. It is a point that we need to start taking far more seriously. Health and care services are already facing unsustainable pressures and without action we are going to see a progressive decline in quality and cost effectiveness.
There is still time to act. Demographic change is happening slowly, it’s predictable and the impact could be mitigated with careful preparation and timely action. It is time to get serious about prevention to improve health and well-being, promote healthy ageing and reduce demand on health and care services. And it is time for a debate about what we want from health and care services in later life and how we make best use of finite resources.
Dr. Richard Harling MBE
Director of Health and Care
Printable version
If you wish to print out this information, please use the document below:
Staffordshire’s ageing population
Our changing populationStaffordshire’s population is getting older. Between 2001 and 2021 the population grew by 70,000 and by 2041 we can expect it to grow by another 80,000. Almost all of this growth is people aged 65 and over, and especially people aged 85 and over, as shown in Figure 1.
Figure 1: historic and projected population growth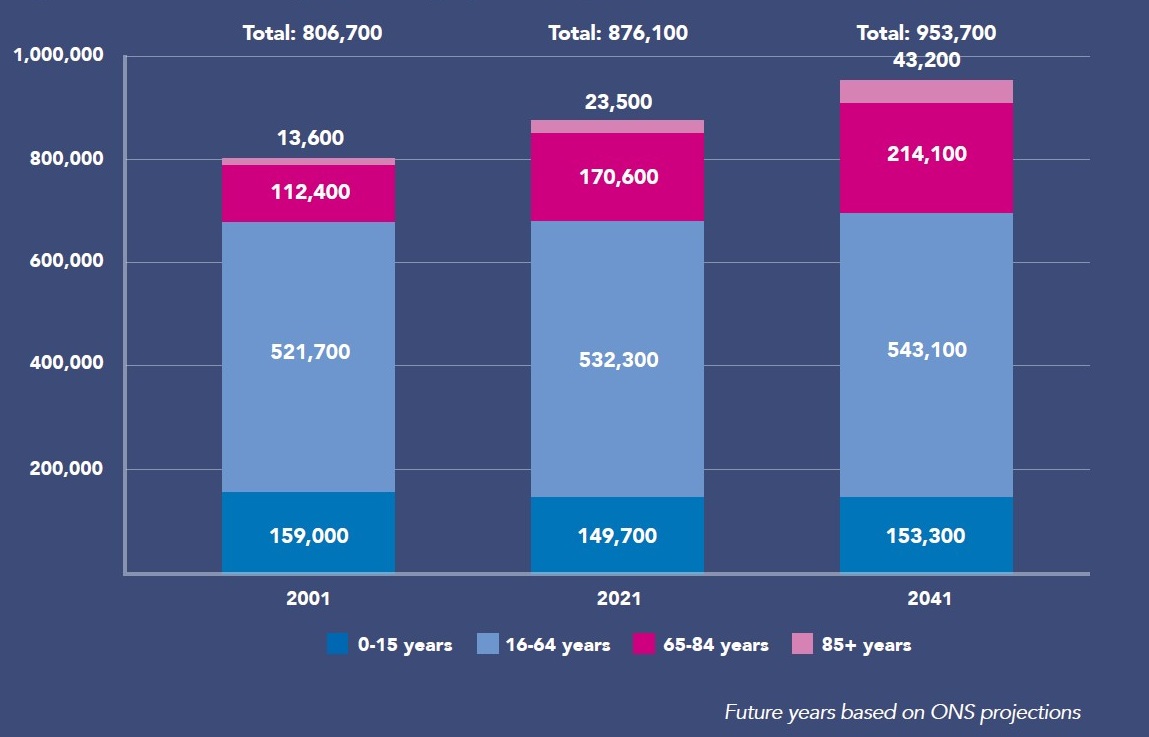
The proportion of the population aged 65 and over will almost double from 15.6% in 2001 to 27.0% by 2041. The proportion of the population aged 85 and over will almost triple from 1.7% in 2001 to 4.5% by 2041.
This will lead to a decrease in the ratio of working age to pension age adults: from 3.4:1 in 2001 to 2.4:1 by 2041, even after taking into account the rise in the state pension age, as shown in Figure 2. On current trends the number of economically-active working age adults for each pension age adult will be even lower, just 2.0:1 by 2041 because only 85% of working age adults are available for work.
Figure 2: ratio of working age to pension age adults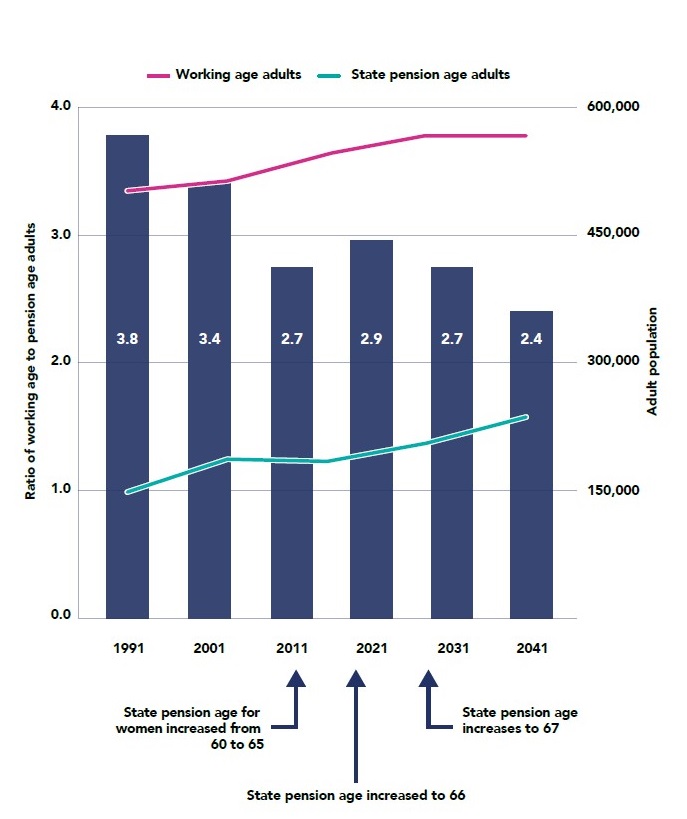
The Government’s scope to raise retirement age further is limited by the fact that it is already higher than healthy life expectancy.
Life expectancy
Life expectancy was rising gradually prior to Covid, however healthy life expectancy had plateaued and was starting to fall, even before the pandemic. There is some uncertainty about projections of life expectancy and healthy life expectancy over the next 20 years. Best estimates on current trends are that life expectancy will continue to rise slowly but healthy life expectancy will fall slightly. This means that by 2041 whilst people may be living a bit longer, any extra years gained will be marred by living with one or more significant illnesses, as shown in Figure 3.
Figure 3: Historic and projected life expectancy
This means that the total burden of ill-health will increase, with more people living with long-term conditions such as diabetes, cancer, dementia and mental health problems. By 2041 around 1 in 5 adults are projected to be living with one or more significant illnesses compared to 1 in 6 currently. Many of these are associated with a range of modifiable risk factors such as obesity, inactivity and social isolation.
Impact on health and care services
The ageing population and more people living with long term conditions will lead to rising demand for health and care services. This will place pressure on funding and on the health and care workforce.
In 2023/24 the NHS spent around £1,875 million in Staffordshire and the County Council around £280 million net on adult social care, including Government Grants. Many people fund their own adult social care.
Health and care expenditure rises steeply with age. NHS expenditure per head of population annually was around £1,500 for adults aged 30 to 64, nearly £3,500 for adults aged 65 to 84 and more than £7,000 for adults aged 85 and over in 2023/24. Staffordshire County Council expenditure for adult social care per head of population annually was around £200 for adults aged 30 to 64, £600 for adults aged 65 to 84 and more than £2,000 for adults aged 85 and over.
A population-based estimate of how public expenditure on health and care services is likely to increase as the population ages is shown in Table 1. This suggests that expenditure can be expected to increase by £310 million by 2041.
There are currently around 21,000 filled posts in the NHS in Staffordshire and another 21,000 in adult social care. Together this is around 7.8% of the working age population working in health and care services; 9.2% of the economically active population.
| Age group | Approximate NHS Spend 2023/24 - NHS | Approximate NHS Spend 2023/24 - Adult Social Care | Change in population - 2031 | Change in population - 2041 |
|---|
| >85 |
£187,500 |
£56,000 |
8,300 (31.7%) |
17,100 (65.4%) |
| 65-84 |
£600,000 |
£112,000 |
21,100 (11.9%) |
36,000 |
| 30-64 |
656,250 |
£87,000 |
-2,500 (-0.6%) |
-1,500 (-0.3%) |
| 0-29 |
£431,250 |
£25,000 |
50 (0.02%) |
6,800 (2.4%) |
| Age group | Growth in spend 2031 - NHS | Growth in spend 2031 - Adult Social Care | Growth in spend 2041 - NHS | Growth in spend 2041 - Adult Social Care |
|---|
| >85 |
£59,528 |
£17,779 |
£122,711 |
£36,650 |
| 65-84 |
£71,213 |
£13,293 |
£117,678 |
£22,659 |
| 30-64 |
-£4,106 |
-£544 |
£1,858 |
-£246 |
| 0-29 |
£70 |
£4 |
£10,258 |
£595 |
| All |
£126,705 |
£30,532 |
£252,505 |
£59,658 |
Using the population-based estimates and assuming the same increases in workforce as in expenditure the total number of health and care posts required can be expected to increase by 3,500 by 2031 and 7,000 by 2041.
Separate workforce-based estimates from the NHS workforce plan and social care workforce strategy suggest bigger increases in the staffing required: a total of 25,000 (60%) additional posts by 2041 as shown in Table 2.
Table 2: workforce-based estimates of staffing requirements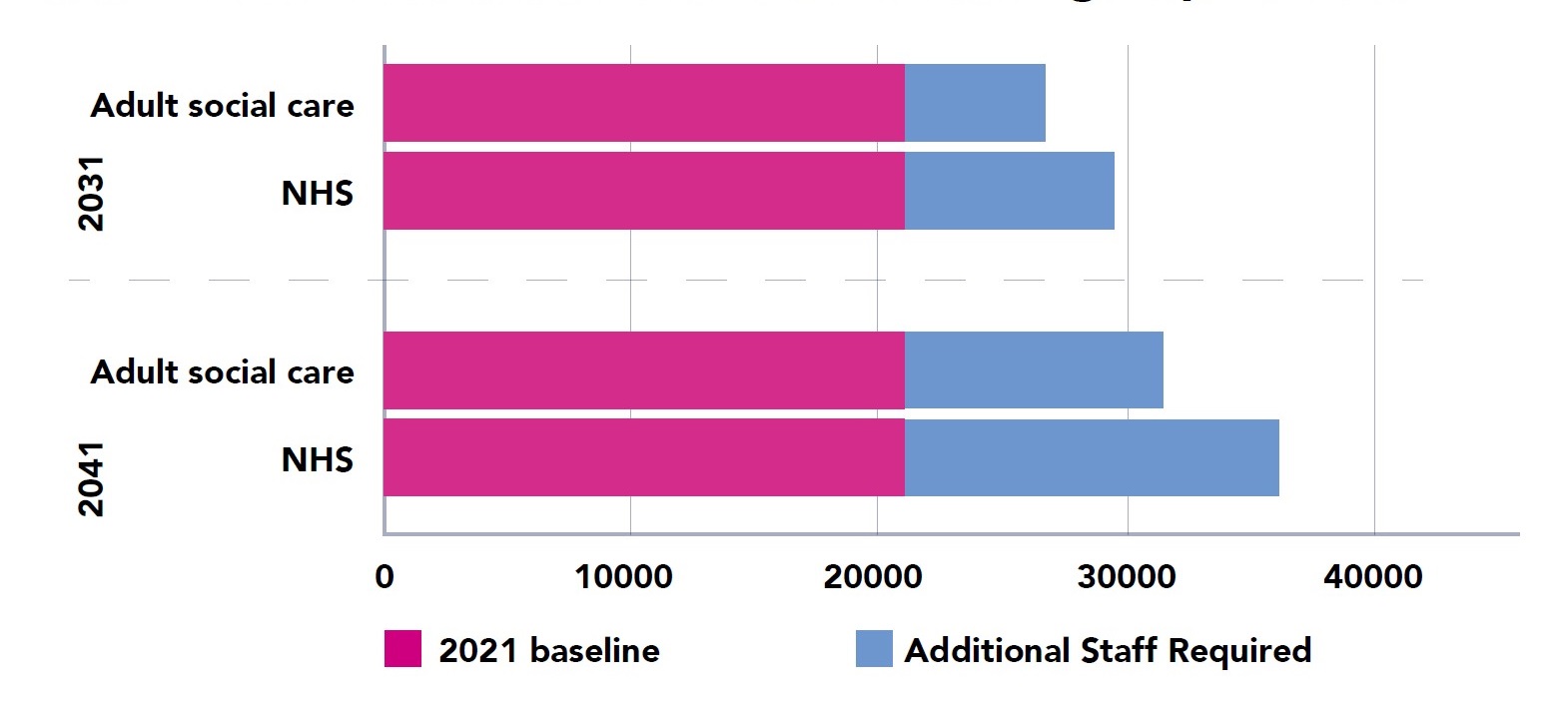
Using the workforce-based estimates and assuming the same increases in expenditure as in workforce suggests bigger increases in the extra funding required: an extra £380 million by 2031 and £763 million by 2041.
Predicting future funding and workforce requirements is difficult. The population and workforce-based estimates represent a reasonable range and I have chosen headline figures somewhere in the middle for the purpose of illustrating the point that the numbers are likely to be significant. Note that future expenditure estimates do not include inflation, which over a 20-year period at 3% would be another £1.8 billion annually.
The challenge
If health and care services continue as now, then by 2041 we will need an extra £600 million and 20,000 additional staff to provide for the ageing population.
This is likely to be challenging. With the working age population more or less static over the next 20 years there are not going to be lots of additional people to pay the extra taxes required to increase funding. This means that each individual of working age will have to pay more. Will the current generation of young adults be able and willing to pay the extra for the care of their parents and grandparents? We don’t know.
Even if the extra funding is available, workforce is likely to remain a challenge. Health and care services are already experiencing difficulties with recruitment and retention. The nursing vacancy rate in England is 10%, there is a shortage of around 6700 GPs nationally, and nearly 10% of adult social care posts in Staffordshire are unfilled.
Filling even more posts will be difficult as the ratio of working age to pension age adults decreases. Another 20,000 posts would take the total to 12.2% of the working age population working in health and care services – and 14.4% of the economically-active population. Is this possible – of course; is it likely – we can’t be sure.
There is therefore a risk that health and care services either run out of money or run out of staff – or both.
A call for action
The good news is that there is still time to act to mitigate this risk.
Healthy ageing
Our first opportunity is a focus on prevention to increase healthy life expectancy. This would have a double benefit: reducing the number of people living with one or more significant illnesses and increasing the workforce who could potentially support them. And we need to start in childhood: the factors that shape our health start from an early age.
There is much we can all do to improve health and well being and promote healthy ageing.
For individuals, regular exercise, a good diet, staying connected, lifelong learning and preparing for later life are my top five tips.
Businesses can do their bit by valuing the health of their employees; communities and the voluntary sector can play a part by supporting older people to maintain their well being and independence.
The public sector has a crucial role: shaping an environment and housing that is conducive to better health and suitable for older people, building and harnessing the strengths of individuals and communities, supporting carers, and making sure that everyone can access services.
Staffordshire has a range of prevention initiatives already underway. We are already working to try and introduce Health in All Policies and we have developed a Healthy Ageing Strategy to support people to remain healthy and independence for as long as possible. Some case studies will accompany this report on the County Council website Director of Public Health annual reports - Staffordshire County Council.
Key to our success will be that national policymakers set the right context for local action by placing as much priority on a long-term strategy for better health as they have done on day-to-day NHS operational issues.
Health and care improvement and reform
Our second opportunity is to rethink the way we care for the older people, especially as they become very elderly and frail towards the end of life.
The current model of care is largely reactive and highly medicalised: we wait for people to get ill and then try to fix them. As we age, we are admitted to hospital with increasing frequently; each admission offers less and less benefit and causes more and more distress. A quarter of hospital beds are occupied by people with less than a year to live and half of deaths occur in hospital.
We instead need a model of care that is proactive and compassionate. Very few of us want to end our days in a hospital or a care home. We need doctors, nurses and social workers to help us explore our options and articulate our wishes as we get older, to anticipate and avoid problems, and to understand that there comes a point when quality of life is more important than quantity of life. This would offer greater dignity for people in their final years and be less resource intensive.
Advances in technology could assist by freeing up time for the health and care workforce. Artificial intelligence could enable people to manage their own health and find support, as well as aid diagnosis and assessments. A range of internet connected devices could help people remain independent in their own homes and provide early alerts to signs of impending health crises.
None of this is to suggest that we do not need to continue our efforts to attract and keep staff. Health and care does offer some of the most rewarding careers available and both the NHS and the County Council have workforce strategies which include recruitment and retention.
These will need to take into account the changing role of staff in a new model of care: to provide preventative and compassionate community-based support rather than hospital-based treatment and develop the skills they will need to take advantage of new technologies.
Recommendations
- Organisations in Staffordshire should consider the impact of an ageing population in all of their strategies, policies and services.
- Individuals and organisations in Staffordshire should consider what they can to do. There is much we can all do to improve health and well-being and promote healthy ageing.
- Public sector partners in Staffordshire should make sure that prevention initiatives have the commitment and resources they need to succeed.
- Government and the NHS nationally and locally should rebalance priorities and funding to improving health and well-being rather than treating disease.
- The Integrated Commissioning Board and local NHS Trusts, supported by NHS England, should reflect on clinical culture and practice and work towards a more proactive and compassionate model of care for older people that offers support in the community and dignity at end of life.
- Organisations in Staffordshire should embrace and explore the potential of technology to promote well being and independence.
- The NHS, County Council and adult social care providers should continue efforts to recruit and retain staff and ensure that they have the right culture and skills